Short summary: The Brain Gauge methods predicted GABA deficits in autism that were later validated with medical imaging.
After having many discussions with lots of people who are interested in the Brain Gauge technology, I became increasingly aware that a vast majority assume that the Brain Gauge was designed and is only used for assessing traumatic brain injury (TBI) or concussion and nothing else. Although we have received support from the Office of Naval Research for the development of the Brain Gauge as a standardized concussion tool, we actually started the development of the device as a means for studying alterations in brain health, and the first funded projects that we were awarded for were in the field of Autism research. The US Army sponsored one of our first projects, and this funded our efforts for building the precursor to the Brain Gauge (the first one weighed in at over 15 lbs even though it was the world’s first portable tactile stimulator!).
Some of my previous research had to do with the investigation of minicolumns – the smallest functional unit in the cortex – and how the organizational scheme created by minicolumnar structure impacted information processing in the cortex. There was a good bit of research on that particular topic in the autism field, as a scientist named Manuel Casanova (you can see his website here https://corticalchauvinism.com/ ) had discovered significant differences in the organization of minicolumns in individuals with autism. His studies utilized post-mortem histology, and he showed that there were 30% more minicolumns in individuals with autism than people without autism. A sample of his work is pictured below:
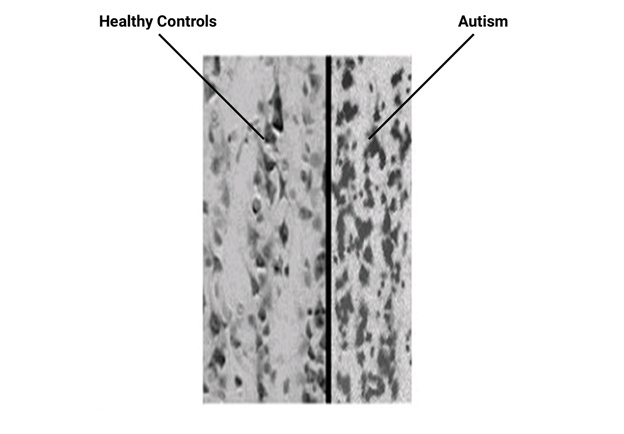
These are histological sections (stained for cell bodies) of controls on the left and autism on the right. Note the higher density of the vertical arrays of cells on the right side. This finding led us to design some sensory tasks to demonstrate that sensory percept would be altered in autism. To summarize, we found that the test results were consistent with the idea (1) that individuals with autism were functionally impacted by the higher density of minicolumns in a positive manner and (2) that interactions between minicolumns were significantly altered in a negative or developmentally disabled manner. It was speculated that this increased density of minicolumns came at a cost – that is, because the cells were so tightly packed (and in a less organized manner) the connections between the minicolumns were disrupted. In particular, the inhibitory connections, or those mediated by GABA (the primary inhibitory neurotransmitter in the cortex), were impacted.
One thing that we found in our initial study was that plasticity of the individual with autism was significantly impacted and this was consistent with the idea that GABA deficits could play a significant role in the disorder.
In order to standardize the testing a bit better, we developed some new tasks that focused on the subject’s ability to adapt to a stimulus. Adaptation is very sensitive to GABA deficits and your ability to adapt to a stimulus is synonymous with plasticity (you can read more about that here: https://insights.corticalmetrics.com/plasticity-measure/ ).
We found some significant differences between our control subjects and our autism subjects. To summarize, this is a summary bar chart of what we found with adults with autism:
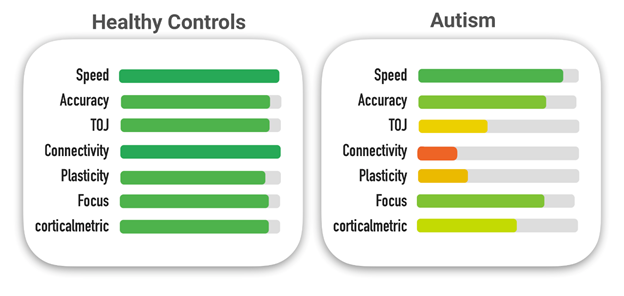
Since our initial study, many other researchers have adopted the Brain Gauge methods for studying autism and in particular, adolescents with autism. The plasticity deficit has been consistently found and reported in other studies and that measure has also been correlated with GABA deficits with MRS imaging (you can read that Puts et al 2016 study here: https://downloads.corticalmetrics.com/pub/puts_reduced_2016.pdf )
What that correlation means is that there is less GABA in the individual with autism, and that the less there is, the lower their plasticity score is.
The feedforward inhibition metric in autism is also well below normal (more details on this in a later post), and this hints that not only is there an inhibitory deficit due to low GABA, but that it is probably a GABAb deficit (two types of GABA in the brain: GABAa and GABAb; another article will detail this, but if you want to read about it in the scientific paper you can do so in Favorov et al 2017 ). There are currently no methods for differentiating GABAa vs. GABAb in the living human cortex, although this information could be very significant for guiding treatment. We believe that this highlights the importance of these types of methods that you can perform with the Brain Gauge and we will continue to pursue this line of research with our collaborators.
Interested in reading more? The Brain Gauge has taken part in quite a few autism studies and if you would like to read them, you can find them by going to www.corticalmetrics.com/publications and typing “autism” in the search bar.